椎间盘性背痛是一个涉及多因素的极其复杂的问题,对医师的诊断及治疗具有挑战性。 在整个过程早期就需要对病理,患者预期以及治疗目标有清晰的理解。
患者在椎间盘退行性疾病的早期(如有早期或无退行性改变)常对多学科方法的保守治疗(镇痛药,物理疗法,治疗性针刺选择)反应良好。 多数椎间盘性背痛的急性加重可在4周内缓解。[93]Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002 Feb;52(475):119-23.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1314232/pdf/11887877.pdfhttp://www.ncbi.nlm.nih.gov/pubmed/11887877?tool=bestpractice.com 经过或未经治疗,约90%的患者在起病后3个月内症状消失。[4]Andersson GB. Epidemiological features of chronic low back pain. Lancet. 1999 Aug 14;354(9178):581-5.http://www.ncbi.nlm.nih.gov/pubmed/10470716?tool=bestpractice.com 仅有小部分 (5%) 腰痛 (LBP) 急性发作患者发生慢性腰痛及相关残疾。[94]Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006 Jun 17;332(7555):1430-4.http://www.bmj.com/content/332/7555/1430?view=long&pmid=16777886http://www.ncbi.nlm.nih.gov/pubmed/16777886?tool=bestpractice.com
当非手术方法证实无效时,建议转诊至外科。 外科治疗是否成功,很大程度上取决于确定该病理及特异性疼痛源是否适合外科治疗。
在现有慢性背痛急性加重时,医师应当找出导致急性症状的原因。 有必要排除导致急性症状的其他原因,如椎间盘炎。
神经急症
怀疑马尾综合征应将患者紧急转诊至医院。 马尾综合征包括鞍区(会阴部)麻痹,括约肌功能不全,尿潴留以及下肢肌力减弱。 症状出现后48小时内需行紧急椎管减压。
椎间盘压迫所致疼痛性神经根障碍(与伴疼痛的运动障碍在同一皮节)适合手术治疗。 这应该与无痛性神经障碍(如无痛性足下垂)及周围神经病变相鉴别。
药物治疗
对乙酰氨基酚经常用于轻度或中度疼痛,因为与非甾体抗炎药 (NSAID) 相比,它更安全。[95]Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007 Oct 2;147(7):505-14.http://www.annals.org/content/147/7/505.fullhttp://www.ncbi.nlm.nih.gov/pubmed/17909211?tool=bestpractice.com 口服非甾体抗炎药常用且对于急性腰痛患者的症状缓解有效。[96]van Tulder MW, Scholten RJ, Koes BW, et al. Nonsteroidal anti-inflammatory drugs for low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group Cochrane review. Spine. 2000 Oct 1;25(19):2501-13.http://www.ncbi.nlm.nih.gov/pubmed/11013503?tool=bestpractice.com [  ]What are the effects of topical NSAIDS in adults with acute musculoskeletal pain?https://cochranelibrary.com/cca/doi/10.1002/cca.1129/full显示答案未发现某种特定非甾体抗炎药比另外一种更有效。[97]Roelofs PD, Deyo RA, Koes BW, et al. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD000396.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000396.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/18253976?tool=bestpractice.com 非甾体抗炎药只能应用有限的时间(不超过 3 个月)。对于长期应用非甾体抗炎药治疗的患者,应当考虑胃粘膜保护,例如使用质子泵抑制剂,尤其对于消化道出血风险更高者(例如老年人)。[6]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. November 2016 [internet publication].https://www.nice.org.uk/guidance/NG59
]What are the effects of topical NSAIDS in adults with acute musculoskeletal pain?https://cochranelibrary.com/cca/doi/10.1002/cca.1129/full显示答案未发现某种特定非甾体抗炎药比另外一种更有效。[97]Roelofs PD, Deyo RA, Koes BW, et al. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD000396.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000396.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/18253976?tool=bestpractice.com 非甾体抗炎药只能应用有限的时间(不超过 3 个月)。对于长期应用非甾体抗炎药治疗的患者,应当考虑胃粘膜保护,例如使用质子泵抑制剂,尤其对于消化道出血风险更高者(例如老年人)。[6]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. November 2016 [internet publication].https://www.nice.org.uk/guidance/NG59
急性症状也可以通过局部镇痛治疗。[98]Jorge LL, Feres CC, Teles VE. Topical preparations for pain relief: efficacy and patient adherence. J Pain Res. 2010 Dec 20;4:11-24.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3048583http://www.ncbi.nlm.nih.gov/pubmed/21386951?tool=bestpractice.com 辣椒素可减少局部P物质,其与介导毒性刺激源有关。[99]Anand P, Bley K. Topical capsaicin for pain management: therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch. Br J Anaesth. 2011 Oct;107(4):490-502.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169333http://www.ncbi.nlm.nih.gov/pubmed/21852280?tool=bestpractice.com 对于肌肉原因引起的疼痛,局部应用非甾体抗炎药可能有效果。 [  ]What are the effects of topical NSAIDS in adults with acute musculoskeletal pain?https://cochranelibrary.com/cca/doi/10.1002/cca.1129/full显示答案局部有限的吸收有助于缓解源于关节周围结构的症状,全身性吸收将治疗药物输送至囊内结构。[100]Derry S, Moore RA, Gaskell H, et al. Topical NSAIDs for acute musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015 Jun 11;(6):CD007402.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007402.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/26068955?tool=bestpractice.com 局部吸收后,血清浓度常小于口服后的浓度5%,因此,对比全身应用的非甾体抗炎药,疗效更加有限。 然而,局部应用非甾体抗炎药可限制全身不良事件的发生。[100]Derry S, Moore RA, Gaskell H, et al. Topical NSAIDs for acute musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015 Jun 11;(6):CD007402.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007402.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/26068955?tool=bestpractice.com
]What are the effects of topical NSAIDS in adults with acute musculoskeletal pain?https://cochranelibrary.com/cca/doi/10.1002/cca.1129/full显示答案局部有限的吸收有助于缓解源于关节周围结构的症状,全身性吸收将治疗药物输送至囊内结构。[100]Derry S, Moore RA, Gaskell H, et al. Topical NSAIDs for acute musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015 Jun 11;(6):CD007402.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007402.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/26068955?tool=bestpractice.com 局部吸收后,血清浓度常小于口服后的浓度5%,因此,对比全身应用的非甾体抗炎药,疗效更加有限。 然而,局部应用非甾体抗炎药可限制全身不良事件的发生。[100]Derry S, Moore RA, Gaskell H, et al. Topical NSAIDs for acute musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015 Jun 11;(6):CD007402.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007402.pub3/fullhttp://www.ncbi.nlm.nih.gov/pubmed/26068955?tool=bestpractice.com
阿片类镇痛药可谨慎应用于严重致残性疼痛且使用乙酰氨基酚和/或非甾体抗炎药无法控制(或不可能控制)的患者。[6]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. November 2016 [internet publication].https://www.nice.org.uk/guidance/NG59 不应当使用阿片类药物治疗慢性腰痛患者。[6]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. November 2016 [internet publication].https://www.nice.org.uk/guidance/NG59[101]Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA. 2018 Mar 6;319(9):872-82.https://jamanetwork.com/journals/jama/fullarticle/2673971http://www.ncbi.nlm.nih.gov/pubmed/29509867?tool=bestpractice.com
肌松剂,如地西泮,是短期缓解急性腰痛的一个选择;然而,因为具有发生副反应(主要是镇静)和药物依赖的风险,需要谨慎应用。[102]van Tulder MW, Touray T, Fulan AD, et al. Muscle relaxants for nonspecific low back pain. Cochrane Database Syst Rev. 2003;(2):CD004252.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004252/fullhttp://www.ncbi.nlm.nih.gov/pubmed/12804507?tool=bestpractice.com
抗抑郁药最常用于慢性腰痛。研究表明,三环类抗抑郁药可缓解症状,而选择性 5-羟色胺再摄取抑制剂则不能。[103]Staiger TO, Gaster B, Sullivan MD, et al. Systematic review of antidepressants in the treatment of chronic low back pain. Spine (Phila Pa 1976). 2003 Nov 15;28(22):2540-5.http://www.ncbi.nlm.nih.gov/pubmed/14624092?tool=bestpractice.com 阿米替林对于改善睡眠质量及解决神经病变性疼痛有效。
对于慢性神经根性疼痛患者,使用加巴喷丁和普瑞巴林可能缓解疼痛,并改善生活质量,[104]Yildirim K, Deniz O, Gureser G, et al. Gabapentin monotherapy in patients with chronic radiculopathy: the efficacy and impact on life quality. J Back Musculoskelet Rehabil. 2009;22(1):17-20.http://www.ncbi.nlm.nih.gov/pubmed/20023359?tool=bestpractice.com[105]Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007 Oct;20(5):456-72.http://www.ncbi.nlm.nih.gov/pubmed/17873599?tool=bestpractice.com 但关于其有效性仍存在争议,需要引起注意。[106]Enke O, New HA, New CH, et al. Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis. CMAJ. 2018 Jul 3;190(26):E786-93.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6028270/http://www.ncbi.nlm.nih.gov/pubmed/29970367?tool=bestpractice.com 普瑞巴林似乎比加巴喷丁的依从性和生物有效性更好。
物理治疗
对于急性腰痛的治疗推荐保持活动,而非卧床休息。[107]Hagen KB, Jamtvedt G, Hilde G, et al. The updated Cochrane review of bed rest for low back pain and sciatica. Spine (Phila Pa 1976). 2005 Mar 1;30(5):542-6.http://www.ncbi.nlm.nih.gov/pubmed/15738787?tool=bestpractice.com[108]Hayden JA, van Tulder MW, Malmivaara A, et al. Exercise therapy for the treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005 Jul 20;(3):CD000335.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000335.pub2/fullhttp://www.ncbi.nlm.nih.gov/pubmed/16034851?tool=bestpractice.com 患者教育(如同背痛学校开展的),学习休息,活动时的体位以及正确的上举技巧,均可改善短期及中期疗效。[109]Heymans MW, van Tulder MW, Esmail R, et al. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976). 2005 Oct 1;30(19):2153-63.http://www.ncbi.nlm.nih.gov/pubmed/16205340?tool=bestpractice.com[110]Heymans MW, de Vet HC, Bongers PM, et al. The effectiveness of high-intensity versus low-intensity back schools in an occupational setting: a pragmatic randomized controlled trial. Spine (Phila Pa 1976). 2006 May 1;31(10):1075-82.http://www.ncbi.nlm.nih.gov/pubmed/16648740?tool=bestpractice.com
轴性症状更像是肌肉性的,因此可用物理疗法干预。 加强力量练习(腹壁及腰肌)的治疗被证实对于轴性疼痛患者具有积极效果。[111]Dickerman RD, Zigler JE. Disocgenic back pain. In: Spivak JM, Connolly PJ, eds. Orthopaedic Knowledge Update: Spine. 3rd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2006:319-30. 然而,练习的时间点具有争论,练习课程在亚急性(2-6周后)和慢性疾病中最有效。 有些练习方案被应用。 McKenzie法是治疗师主导的用于评估和分类患者并制定具体练习的系统。[112]Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50(4):209-16.https://ac.els-cdn.com/S0004951414601100/1-s2.0-S0004951414601100-main.pdf?_tid=99aa8043-54c9-4d08-853f-eb39601c6c2d&acdnat=1544532510_9ea0b54ccfd9b965f168a8a6fc2d1314http://www.ncbi.nlm.nih.gov/pubmed/15574109?tool=bestpractice.com McKenzie法比非特异性的,通用的指南具有更好的短期效果,并且与加强力量和稳定性的方案具有相同的结果。[112]Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50(4):209-16.https://ac.els-cdn.com/S0004951414601100/1-s2.0-S0004951414601100-main.pdf?_tid=99aa8043-54c9-4d08-853f-eb39601c6c2d&acdnat=1544532510_9ea0b54ccfd9b965f168a8a6fc2d1314http://www.ncbi.nlm.nih.gov/pubmed/15574109?tool=bestpractice.com[113]May S, Donelson R. Evidence-informed management of chronic low back pain with the McKenzie method. Spine J. 2008 Jan-Feb;8(1):134-41.http://www.ncbi.nlm.nih.gov/pubmed/18164461?tool=bestpractice.com
脊柱推拿对于治疗急性腰痛与物理疗法疗效类似。[114]Cherkin DC, Deyo RA, Battié M, et al. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998 Oct 8;339(15):1021-9.http://www.nejm.org/doi/full/10.1056/NEJM199810083391502#t=articlehttp://www.ncbi.nlm.nih.gov/pubmed/9761803?tool=bestpractice.com[115]Rubinstein SM, Terwee CB, Assendelft WJ, et al. Spinal manipulative therapy for acute low-back pain. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD008880.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008880.pub2/fullhttp://www.ncbi.nlm.nih.gov/pubmed/22972127?tool=bestpractice.com
有许多干扰系统及刺激物可能有益于急性或慢性神经根性疼痛;然而,对于它们的应用尚存争议。[116]Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007 Oct 2;147(7):492-504.http://www.annals.org/content/147/7/492.longhttp://www.ncbi.nlm.nih.gov/pubmed/17909210?tool=bestpractice.com[117]Hurley DA, McDonough SM, Dempster M, et al. A randomized clinical trial of manipulative therapy and interferential therapy for acute low back pain. Spine (Phila Pa 1976). 2004 Oct 15;29(20):2207-16.http://www.ncbi.nlm.nih.gov/pubmed/15480130?tool=bestpractice.com
无论是预防还是治疗腰痛,支具的应用都是无效的。[118]Jellema P, van Tulder MW, van Poppel MN, et al. Lumbar supports for prevention and treatment of low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine. 2001 Feb 15;26(4):377-86.http://www.ncbi.nlm.nih.gov/pubmed/11224885?tool=bestpractice.com 牵引在过去曾被用作腰痛治疗的方法。 然而,最近更多的研究表明,没有证据表明其优于静息疗法(卧床休息)。[119]Luijsterburg PA, Verhagen AP, Ostelo RW, et al. Physical therapy plus general practitioners' care versus general practitioners' care alone for sciatica: a randomised clinical trial with a 12-month follow-up. Eur Spine J. 2008 Apr;17(4):509-17.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2295266/?tool=pubmedhttp://www.ncbi.nlm.nih.gov/pubmed/18172697?tool=bestpractice.com[120]Luijsterburg PA, Verhagen AP, Ostelo RW, et al. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spin J. 2007 Jul;16(7):881-99.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219647/?tool=pubmedhttp://www.ncbi.nlm.nih.gov/pubmed/17415595?tool=bestpractice.com
替代疗法
一些疗法可在传统疗法基础上应用,或作为替代疗法应用。
可以考虑使用非药物疗法(例如针灸、指压按摩和瑜伽)。[121]Saper RB, Lemaster C, Delitto A, et al. Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Ann Intern Med. 2017 Jul 18;167(2):85-94.http://www.ncbi.nlm.nih.gov/pubmed/28631003?tool=bestpractice.com[116]Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007 Oct 2;147(7):492-504.http://www.annals.org/content/147/7/492.longhttp://www.ncbi.nlm.nih.gov/pubmed/17909210?tool=bestpractice.com
治疗性穿刺选择
选择性神经根阻滞
硬膜外注射
通过长效局部麻醉药浸润,加入或不加入局部糖皮质激素后,可有效治疗多水平,双侧病变的神经根性疼痛。 系统评价和多项研究发现,有良好的证据证明,硬膜外注射(使用尾椎和腰椎椎板间途径)可短期和/或长期缓解继发于椎间盘突出和神经根炎的慢性疼痛。[122]Parr AT, Manchikanti L, Hameed H, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012 May-Jun;15(3):E159-98.http://www.ncbi.nlm.nih.gov/pubmed/22622911?tool=bestpractice.com[123]Benyamin RM, Manchikanti L, Parr AT, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012 Jul-Aug;15(4):E363-404.http://www.ncbi.nlm.nih.gov/pubmed/22828691?tool=bestpractice.com[124]Benoist M, Boulu P, Hayem G. Epidural steroid injections in the management of low-back pain with radiculopathy: an update of their efficacy and safety. Eur Spine J. 2012 Feb;21(2):204-13.http://www.ncbi.nlm.nih.gov/pubmed/21922288?tool=bestpractice.com[125]Bicket MC, Horowitz JM, Benzon HT, et al. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. Spine J. 2015 Feb 1;15(2):348-62.http://www.ncbi.nlm.nih.gov/pubmed/25463400?tool=bestpractice.com[126]Chou R, Hashimoto R, Friedly J, et al. Epidural corticosteroid injections for radiculopathy and spinal stenosis: a systematic review and meta-analysis. Ann Intern Med. 2015 Sep 1;163(5):373-81.http://www.ncbi.nlm.nih.gov/pubmed/26302454?tool=bestpractice.com[127]Manchikanti L, Benyamin RM, Falco FJ, et al. Do epidural injections provide short- and long-term relief for lumbar disc herniation? a systematic review. Clin Orthop Relat Res. 2015 Jun;473(6):1940-56.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4419020/http://www.ncbi.nlm.nih.gov/pubmed/24515404?tool=bestpractice.com 已报告的罕见并发症包括,与椎间孔途径相关的截瘫,以及并发脊髓脊神经根动脉破坏。[124]Benoist M, Boulu P, Hayem G. Epidural steroid injections in the management of low-back pain with radiculopathy: an update of their efficacy and safety. Eur Spine J. 2012 Feb;21(2):204-13.http://www.ncbi.nlm.nih.gov/pubmed/21922288?tool=bestpractice.com[128]Spijker-Huiges A, Vermeulen K, Winters JC, et al. Costs and cost-effectiveness of epidural steroids for acute lumbosacral radicular syndrome in general practice: an economic evaluation alongside a pragmatic randomized control trial. Spine (Phila Pa 1976). 2014 Nov 15;39(24):2007-12.http://www.ncbi.nlm.nih.gov/pubmed/25202937?tool=bestpractice.com 有中等程度的证据显示治疗继发于脊柱狭窄的疼痛,无椎间盘突出的轴性疼痛以及术后综合征有效。
药物可以注射入椎间孔或椎管。 通过腰椎途径(通过后纵韧带)或尾部途径(通过骶管裂孔)可向椎管内输注。 需要的注射量随每一途径增加。
尽管对于某些结局指标,硬膜外类固醇注射提供的益处可能大于加巴喷丁,但差异不大,在大多数病例中,都是短暂的。[129]Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ. 2015 Apr 16;350:h1748.http://www.bmj.com/content/350/bmj.h1748.longhttp://www.ncbi.nlm.nih.gov/pubmed/25883095?tool=bestpractice.com
在 2012 年,美国因硬膜外或椎旁注射不含防腐剂的醋酸甲泼尼龙(由一家药物制剂公司生产)而导致出现中枢神经系统真菌感染暴发。[130]Kainer MA, Reagan DR, Nguyen DB, et al; Tennessee Fungal Meningitis Investigation Team. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012 Dec 6;367(23):2194-203.http://www.nejm.org/doi/full/10.1056/NEJMoa1212972http://www.ncbi.nlm.nih.gov/pubmed/23131029?tool=bestpractice.com 尽管极为罕见,但这强调了如果采用这项给药途径,在药物准备及注射过程中必须遵循最严格的标准。
关节突关节阻滞
关节突射频神经切断术
如果轴性背痛持续存在的时间超过 3 个月,并且患者对小关节阻滞治疗急性疼痛有反应,则射频消融可能对小关节源性疼痛产生更长期的疗效,但尚不明确其有效性。[131]Leggett LE, Soril LJ, Lorenzetti DL, et al. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag. 2014 Sep-Oct;19(5):e146-53.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4197759/http://www.ncbi.nlm.nih.gov/pubmed/25068973?tool=bestpractice.com[132]Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of radiofrequency denervation on pain intensity among patients with chronic low back pain: the Mint randomized clinical trials. JAMA. 2017 Jul 4;318(1):68-81.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5541325/http://www.ncbi.nlm.nih.gov/pubmed/28672319?tool=bestpractice.com
手术治疗
神经减压
对于急性和慢性神经根性疼痛患者,神经根和神经结构减压是外科干预的重要一部分。
切除部分下关节突,下关节突切削术,或退变关节突关节整体切除可有助于关节下减压并消除一个潜在的疼痛源。
通过放置椎体间内植物以增加椎间盘高度,扩大椎间孔以达到间接减压。
脊柱融合
脊柱融合术的临床指征包括:保守治疗失败,迁延不愈的慢性疼痛,超过 1 年的残疾,以及在磁共振成像显示局限于 1 或 2 个椎间盘水平的进展性椎间盘退行性变。[133]Andersson GB, Shen FH. Operative management of the degenerative disc: posterior and posterolateral procedures. In: Herkowitz HN, Dvorak J, Bell G, et al, eds. The Lumbar Spine. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2004;317-23.[134]Sidhu KS, Herkowitz HN. Spinal instrumentation in the management of degenerative disorders of the lumbar spine. Clin Orthop Rel Res. 1997 Feb;(335):39-53.http://www.ncbi.nlm.nih.gov/pubmed/9020205?tool=bestpractice.com 然而,由于腰痛的多因素性以及脊柱融合术的成功率有限且不一致,手术指征依不同的国家及外科医师而不同。[135]Fritzell P, Hagg O, Wessberg P, et al. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976). 2001 Dec 1;26(23):2521-32; discussion 2532-4.http://www.ncbi.nlm.nih.gov/pubmed/11725230?tool=bestpractice.com对于存在明显失稳的明确病变(峡部裂,峡部脊椎前移伴不稳定,关节突关节病合并退行性脊椎前移),在考虑行手术治疗前,给予较短期的(6 个月)物理治疗可能有效。 对于神经根病变的病例,症状超过6个月提示预后不良。[136]Rihn JA, Hilibrand AS, Radcliff K, et al. Duration of symptoms resulting from lumbar disc herniation: effect on treatment outcomes: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am. 2011 Oct 19;93(20):1906-14.http://www.ncbi.nlm.nih.gov/pubmed/22012528?tool=bestpractice.com 类似的,脊柱狭窄患者在症状出现12个月之内治疗,预后较好。[137]Radcliff KE, Rihn J, Hilibrand A, et al. Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes?: analysis of the Spine Outcomes Research Trial. Spine (Phila Pa 1976). 2011 Dec 1;36(25):2197-210.http://www.ncbi.nlm.nih.gov/pubmed/21912308?tool=bestpractice.com 一项系统性综述发现,有症状的腰椎滑脱的运动员手术治疗后5-12个月内,84%恢复其体育运动。[138]Drazin D, Shirzadi A, Jeswani S, et al. Direct surgical repair of spondylolysis in athletes: indications, techniques, and outcomes. Neurosurg Focus. 2011 Nov;31(5):E9.http://thejns.org/doi/full/10.3171/2011.9.FOCUS11180http://www.ncbi.nlm.nih.gov/pubmed/22044108?tool=bestpractice.com
对于患者主诉,预期,生活方式以及任何可能的功能缺失的详细了解,可以通过一些经过认证的评分系统(ODI,Roland Morris,SF36,Nottingham健康档案,疼痛评分,疼痛图表,Zung/MSPQ)获得。 在考虑行任何手术前,可对不合适行为的Wadell征进行临床评价。[139]Waddell G, McCulloch JA, Kummel E, et al. Nonorganic physical signs in low-back pain. Spine (Phila Pa 1976). 1980 Mar-Apr;5(2):117-25.http://www.ncbi.nlm.nih.gov/pubmed/6446157?tool=bestpractice.com[140]Main CJ, Waddell G. Behavioral responses to examination. A reappraisal of the interpretation of "nonorganic signs". Spine (Phila Pa 1976). 1998;23:2367-2371.http://www.ncbi.nlm.nih.gov/pubmed/9820920?tool=bestpractice.com 应该把这些和影像学发现以及推测的导致症状的病理改变结合起来考察。临床医师将这些因素综合考虑后再做融合手术对于好的手术结果十分重要。
脊柱融合手术最基本的目标是阻止疼痛腰椎节段进一步的节段运动。 因此,这一过程对于具有脊柱失稳证据(创伤,肿瘤,感染,畸形,和椎间盘疾病)的患者是最适合的。 因此,这一过程对于具有脊柱失稳证据(创伤,肿瘤,感染,畸形,和椎间盘疾病)的患者是最适合的。对于无明显不稳定的椎间盘退变性疾病,要根据是否预防疼痛椎间盘周围的活动或一并去除椎间盘、融合运动节段将阻止疾病进展并缓解疼痛,来选择脊柱融合手术。[141]Hanley EN Jr, David SM. Lumbar arthrodesis for the treatment of back pain. J Bone Joint Surg Am. 1999 May;81(5):716-30.http://www.ncbi.nlm.nih.gov/pubmed/10360702?tool=bestpractice.com[142]Kishen TJ, Diwan AD. Fusion versus disk replacement for degenerative conditions of the lumbar and cervical spine: quid est testimonium? Orthop Clin North Am. 2010 Apr;41(2):167-81.http://www.ncbi.nlm.nih.gov/pubmed/20399356?tool=bestpractice.com
脊柱融合术最常需要使用移植物来连接融合节段。切除椎间隙并处理终板(有或没有结构支撑)后,将移植物放置在后外侧沟或椎体间。为了提高融合速度,已经使用骨形态发生蛋白。
一些在临床上用于腰椎融合的手术,包括:后外侧融合术(应用或不应用椎弓根螺钉)、后路腰锥体间融合术、经椎间孔腰椎体间融合术,以及前路腰椎体间融合术。一般而言,使用器械可提高融合率,但以并发症发生率、失血增加以及手术时间延长为代价。[135]Fritzell P, Hagg O, Wessberg P, et al. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976). 2001 Dec 1;26(23):2521-32; discussion 2532-4.http://www.ncbi.nlm.nih.gov/pubmed/11725230?tool=bestpractice.com[143]Fritzell P, Hägg O, Wessberg P, et al. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976). 2002 Jun 1;27(11):1131-41.http://www.ncbi.nlm.nih.gov/pubmed/12045508?tool=bestpractice.com 所有的融合技术可以减少疼痛及残疾,也未发现降低手术(适应症)要求有明显的缺点。[143]Fritzell P, Hägg O, Wessberg P, et al. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976). 2002 Jun 1;27(11):1131-41.http://www.ncbi.nlm.nih.gov/pubmed/12045508?tool=bestpractice.com[144]Lee GW, Lee SM, Ahn MW, et al. Comparison of posterolateral lumbar fusion and posterior lumbar interbody fusion for patients younger than 60 years with isthmic spondylolisthesis. Spine (Phila Pa 1976). 2014 Nov 15;39(24):E1475-80.http://www.ncbi.nlm.nih.gov/pubmed/25202935?tool=bestpractice.com[145]Liu XY, Qiu GX, Weng XS, et al. What is the optimum fusion technique for adult spondylolisthesis-PLIF or PLF or PLIF plus PLF? A meta-analysis from 17 comparative studies. Spine (Phila Pa 1976). 2014 Oct 15;39(22):1887-98.http://www.ncbi.nlm.nih.gov/pubmed/25099321?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 椎体滑脱:屈伸位观来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 椎体滑脱:屈伸位观来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术前磁共振成像矢状位T2序列来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术前磁共振成像矢状位T2序列来自N.Quiraishi博士的收集 [Citation ends].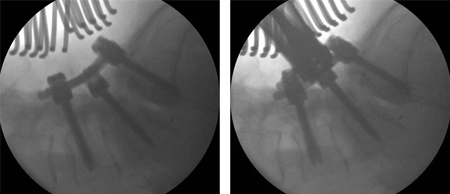 [Figure caption and citation for the preceding image starts]: 术中影像显示畸形逐渐减小:腰4至骶1导航下融合,在腰5骶1经椎间孔融合及腰5双侧减压来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术中影像显示畸形逐渐减小:腰4至骶1导航下融合,在腰5骶1经椎间孔融合及腰5双侧减压来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术后影像来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术后影像来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术前和术后观:一位表现为背痛和神经性跛行的患者腰4-5狭窄及退行性滑脱,腰5骶1椎间盘退变(左,T2加权矢状位磁共振成像);实施了腰4-骶1减压,两个节段的经椎间孔腰椎椎体间融合手术(前后位,上;侧位,下)来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术前和术后观:一位表现为背痛和神经性跛行的患者腰4-5狭窄及退行性滑脱,腰5骶1椎间盘退变(左,T2加权矢状位磁共振成像);实施了腰4-骶1减压,两个节段的经椎间孔腰椎椎体间融合手术(前后位,上;侧位,下)来自N.Quiraishi博士的收集 [Citation ends].
人工椎间盘置换(ADR)
人工椎间盘置换术 (ADR) 是另一种外科技术,不属于常规临床实践,是指完整去除损伤的或变性的椎间盘,并以人工椎间盘代替。  [Figure caption and citation for the preceding image starts]: 椎间盘置换:患者表现为严重的背痛,先前因右侧骶 1 神经根病变已经接受了右侧腰 5 骶 1 椎间盘切除。 尽管初期康复,但右侧骶1疼痛及背痛在10个月后复发。 磁共振成像显示腰5骶1椎间盘退变(左,T2加权矢状位观)。 患者继而接受椎间盘置换术(前后位,右上,侧位,右下)。 背痛及右下肢痛彻底解除来自N.Quiraishi博士的收集 [Citation ends]. 这一装置的目的在于恢复椎间盘正常的动力学特征,缓解疼痛,同时避免失稳,并保护邻近关节突过度退变。置换整个椎间盘的原理是基于设计和用于其他关节(膝和髋关节置换)的类似假体置换取得成功。因此,所用的材料也是类似的(聚乙烯、铬、钴、钛)。人工椎间盘置换的应用指征包括:保守治疗失败;椎间盘退行性疾病致残的腰痛,累及不超过2个椎间盘。[146]Fekete TF, Porchet F. Overview of disc arthroplasty-past, present and future. Acta Neurochir (Wien). 2010 Mar;152(3):393-404.http://www.ncbi.nlm.nih.gov/pubmed/19844656?tool=bestpractice.com 这些指征与脊柱融合的指征相似,但有一些注意事项(相对早期的关节突关节受累,无明显的失稳;如椎体滑脱)。 人工椎间盘置换的禁忌症包括狭窄,关节突关节炎,峡部裂或椎体滑脱,继发于突出椎间盘的神经根病变,硬化,骨质疏松,妊娠,肥胖,感染和骨折。[147]Lin EL, Wang JC. Total disk arthroplasty. J Am Acad Orthop Surg. 2006 Dec;14(13):705-14.http://www.ncbi.nlm.nih.gov/pubmed/17148618?tool=bestpractice.com 人工椎间盘置换与融合手术在疗效和安全性上的对比已经有文献详细报道。 尽管最初的结果鼓励人工椎间盘的应用,[148]Zigler JE. Clinical results with ProDisc: European experience and U.S. investigation device exemption study. Spine. 2003 Oct 15;28(20):S163-6.http://www.ncbi.nlm.nih.gov/pubmed/14560187?tool=bestpractice.com 随访时间更长的较近期研究表明,在 12 个月时,活动性方面的初始获益减少,[149]Delamarter RB, Fribourg DM, Kanim LE, et al. ProDisc artificial total lumbar disc replacement: introduction and early results from the United States clinical trial. Spine. 2003 Oct 15;28(20):S167-75.http://www.ncbi.nlm.nih.gov/pubmed/14560188?tool=bestpractice.com 在手术后 17 年时,完全丧失活动性,导致关节僵硬。[150]Putzier M, Funk JF, Schneider SV, et al. Charité total disc replacement -clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006 Feb;15(2):183-95.http://www.ncbi.nlm.nih.gov/pubmed/16254716?tool=bestpractice.com 关于 ADR 的长期益处和并发症,这些发现给出了一些提醒,尤其是在预防关节僵硬方面,[151]Resnick DK, Watters WC. Lumbar disc arthroplasty: a critical review. Clin Neurosurg. 2007;54:83-7.http://www.ncbi.nlm.nih.gov/pubmed/18504901?tool=bestpractice.com[152]Jacobs WC, van der Gaag NA, Kruyt MC, et al. Total disc replacement for chronic discogenic low back pain: a Cochrane review. Spine (Phila Pa 1976). 2013 Jan 1;38(1):24-36.http://www.ncbi.nlm.nih.gov/pubmed/22996268?tool=bestpractice.com[153]Jacobs W, Van der Gaag NA, Tuschel A, et al. Total disc replacement for chronic back pain in the presence of disc degeneration. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD008326.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008326.pub2/fullhttp://www.ncbi.nlm.nih.gov/pubmed/22972118?tool=bestpractice.com 使得将其作为一种治疗技术应用的普遍性下降。
[Figure caption and citation for the preceding image starts]: 椎间盘置换:患者表现为严重的背痛,先前因右侧骶 1 神经根病变已经接受了右侧腰 5 骶 1 椎间盘切除。 尽管初期康复,但右侧骶1疼痛及背痛在10个月后复发。 磁共振成像显示腰5骶1椎间盘退变(左,T2加权矢状位观)。 患者继而接受椎间盘置换术(前后位,右上,侧位,右下)。 背痛及右下肢痛彻底解除来自N.Quiraishi博士的收集 [Citation ends]. 这一装置的目的在于恢复椎间盘正常的动力学特征,缓解疼痛,同时避免失稳,并保护邻近关节突过度退变。置换整个椎间盘的原理是基于设计和用于其他关节(膝和髋关节置换)的类似假体置换取得成功。因此,所用的材料也是类似的(聚乙烯、铬、钴、钛)。人工椎间盘置换的应用指征包括:保守治疗失败;椎间盘退行性疾病致残的腰痛,累及不超过2个椎间盘。[146]Fekete TF, Porchet F. Overview of disc arthroplasty-past, present and future. Acta Neurochir (Wien). 2010 Mar;152(3):393-404.http://www.ncbi.nlm.nih.gov/pubmed/19844656?tool=bestpractice.com 这些指征与脊柱融合的指征相似,但有一些注意事项(相对早期的关节突关节受累,无明显的失稳;如椎体滑脱)。 人工椎间盘置换的禁忌症包括狭窄,关节突关节炎,峡部裂或椎体滑脱,继发于突出椎间盘的神经根病变,硬化,骨质疏松,妊娠,肥胖,感染和骨折。[147]Lin EL, Wang JC. Total disk arthroplasty. J Am Acad Orthop Surg. 2006 Dec;14(13):705-14.http://www.ncbi.nlm.nih.gov/pubmed/17148618?tool=bestpractice.com 人工椎间盘置换与融合手术在疗效和安全性上的对比已经有文献详细报道。 尽管最初的结果鼓励人工椎间盘的应用,[148]Zigler JE. Clinical results with ProDisc: European experience and U.S. investigation device exemption study. Spine. 2003 Oct 15;28(20):S163-6.http://www.ncbi.nlm.nih.gov/pubmed/14560187?tool=bestpractice.com 随访时间更长的较近期研究表明,在 12 个月时,活动性方面的初始获益减少,[149]Delamarter RB, Fribourg DM, Kanim LE, et al. ProDisc artificial total lumbar disc replacement: introduction and early results from the United States clinical trial. Spine. 2003 Oct 15;28(20):S167-75.http://www.ncbi.nlm.nih.gov/pubmed/14560188?tool=bestpractice.com 在手术后 17 年时,完全丧失活动性,导致关节僵硬。[150]Putzier M, Funk JF, Schneider SV, et al. Charité total disc replacement -clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006 Feb;15(2):183-95.http://www.ncbi.nlm.nih.gov/pubmed/16254716?tool=bestpractice.com 关于 ADR 的长期益处和并发症,这些发现给出了一些提醒,尤其是在预防关节僵硬方面,[151]Resnick DK, Watters WC. Lumbar disc arthroplasty: a critical review. Clin Neurosurg. 2007;54:83-7.http://www.ncbi.nlm.nih.gov/pubmed/18504901?tool=bestpractice.com[152]Jacobs WC, van der Gaag NA, Kruyt MC, et al. Total disc replacement for chronic discogenic low back pain: a Cochrane review. Spine (Phila Pa 1976). 2013 Jan 1;38(1):24-36.http://www.ncbi.nlm.nih.gov/pubmed/22996268?tool=bestpractice.com[153]Jacobs W, Van der Gaag NA, Tuschel A, et al. Total disc replacement for chronic back pain in the presence of disc degeneration. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD008326.https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008326.pub2/fullhttp://www.ncbi.nlm.nih.gov/pubmed/22972118?tool=bestpractice.com 使得将其作为一种治疗技术应用的普遍性下降。
多学科治疗
腰痛保守治疗的趋势为支持采用多学科疗法。[154]Guzmán J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001 Jun 23;322(7301):1511-6.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC33389/?tool=pubmedhttp://www.ncbi.nlm.nih.gov/pubmed/11420271?tool=bestpractice.com[155]Brox JL, Sorensen R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;26:377-86. 这些学科通常包含身体要素,且包括社会,职业以及心理要素。多学科康复比单一康复课程更加有效。[154]Guzmán J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001 Jun 23;322(7301):1511-6.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC33389/?tool=pubmedhttp://www.ncbi.nlm.nih.gov/pubmed/11420271?tool=bestpractice.com
疼痛门诊
多学科门诊由疼痛专科医生(一般是对疼痛管理有兴趣的麻醉科医生)以及专科护士、理疗师、心理学医生和药剂师组成。
目标是简化用药,促进解决人体工程学问题,以及可能有的心理问题。
疼痛科医生可以实施如神经根和硬膜外注射以及关节突射频神经切断术。
功能性/职业性康复
是指为帮助有健康问题的人们回归及保持工作,采取的任何措施。 这是一种途径、干预以及服务,焦点集中在以工作为中心的卫生保健,以及调整工作环境以适应适龄工作者。 已对几个“回归工作”项目进行研究,针对的是提供人工搬运建议及相关辅助设备。[156]Waddell G, Burton AK, Kendall NAS. Vocational rehabilitation: what works, for whom, and when? [internet publication].https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/209474/hwwb-vocational-rehabilitation.pdf 但一篇 Cochrane 评价显示,有中等质量证据表明,与不干预或采用其他干预相比,这些干预并不缓解背痛、背痛相关残疾或误工。[157]Verbeek J, Martimo KP, Karppinen J, et al. Manual material handling advice and assistive devices for preventing and treating back pain in workers: a Cochrane Systematic Review. Occup Environ Med. 2012 Jan;69(1):79-80.http://www.ncbi.nlm.nih.gov/pubmed/21849341?tool=bestpractice.com 还没有随机对照临床试验证据支持 MMH 咨询和训练或 MMH 辅助设备对背痛治疗有效。
 ]未发现某种特定非甾体抗炎药比另外一种更有效。[97] 非甾体抗炎药只能应用有限的时间(不超过 3 个月)。对于长期应用非甾体抗炎药治疗的患者,应当考虑胃粘膜保护,例如使用质子泵抑制剂,尤其对于消化道出血风险更高者(例如老年人)。[6]
]未发现某种特定非甾体抗炎药比另外一种更有效。[97] 非甾体抗炎药只能应用有限的时间(不超过 3 个月)。对于长期应用非甾体抗炎药治疗的患者,应当考虑胃粘膜保护,例如使用质子泵抑制剂,尤其对于消化道出血风险更高者(例如老年人)。[6] ]局部有限的吸收有助于缓解源于关节周围结构的症状,全身性吸收将治疗药物输送至囊内结构。[100] 局部吸收后,血清浓度常小于口服后的浓度5%,因此,对比全身应用的非甾体抗炎药,疗效更加有限。 然而,局部应用非甾体抗炎药可限制全身不良事件的发生。[100]
]局部有限的吸收有助于缓解源于关节周围结构的症状,全身性吸收将治疗药物输送至囊内结构。[100] 局部吸收后,血清浓度常小于口服后的浓度5%,因此,对比全身应用的非甾体抗炎药,疗效更加有限。 然而,局部应用非甾体抗炎药可限制全身不良事件的发生。[100] [Figure caption and citation for the preceding image starts]: 椎体滑脱:屈伸位观来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 椎体滑脱:屈伸位观来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术前磁共振成像矢状位T2序列来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术前磁共振成像矢状位T2序列来自N.Quiraishi博士的收集 [Citation ends].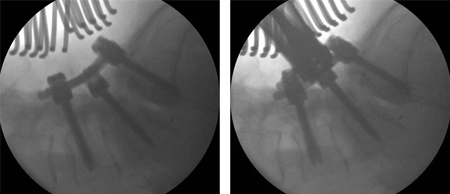 [Figure caption and citation for the preceding image starts]: 术中影像显示畸形逐渐减小:腰4至骶1导航下融合,在腰5骶1经椎间孔融合及腰5双侧减压来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术中影像显示畸形逐渐减小:腰4至骶1导航下融合,在腰5骶1经椎间孔融合及腰5双侧减压来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术后影像来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术后影像来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 术前和术后观:一位表现为背痛和神经性跛行的患者腰4-5狭窄及退行性滑脱,腰5骶1椎间盘退变(左,T2加权矢状位磁共振成像);实施了腰4-骶1减压,两个节段的经椎间孔腰椎椎体间融合手术(前后位,上;侧位,下)来自N.Quiraishi博士的收集 [Citation ends].
[Figure caption and citation for the preceding image starts]: 术前和术后观:一位表现为背痛和神经性跛行的患者腰4-5狭窄及退行性滑脱,腰5骶1椎间盘退变(左,T2加权矢状位磁共振成像);实施了腰4-骶1减压,两个节段的经椎间孔腰椎椎体间融合手术(前后位,上;侧位,下)来自N.Quiraishi博士的收集 [Citation ends]. [Figure caption and citation for the preceding image starts]: 椎间盘置换:患者表现为严重的背痛,先前因右侧骶 1 神经根病变已经接受了右侧腰 5 骶 1 椎间盘切除。 尽管初期康复,但右侧骶1疼痛及背痛在10个月后复发。 磁共振成像显示腰5骶1椎间盘退变(左,T2加权矢状位观)。 患者继而接受椎间盘置换术(前后位,右上,侧位,右下)。 背痛及右下肢痛彻底解除来自N.Quiraishi博士的收集 [Citation ends]. 这一装置的目的在于恢复椎间盘正常的动力学特征,缓解疼痛,同时避免失稳,并保护邻近关节突过度退变。置换整个椎间盘的原理是基于设计和用于其他关节(膝和髋关节置换)的类似假体置换取得成功。因此,所用的材料也是类似的(聚乙烯、铬、钴、钛)。人工椎间盘置换的应用指征包括:保守治疗失败;椎间盘退行性疾病致残的腰痛,累及不超过2个椎间盘。[146] 这些指征与脊柱融合的指征相似,但有一些注意事项(相对早期的关节突关节受累,无明显的失稳;如椎体滑脱)。 人工椎间盘置换的禁忌症包括狭窄,关节突关节炎,峡部裂或椎体滑脱,继发于突出椎间盘的神经根病变,硬化,骨质疏松,妊娠,肥胖,感染和骨折。[147] 人工椎间盘置换与融合手术在疗效和安全性上的对比已经有文献详细报道。 尽管最初的结果鼓励人工椎间盘的应用,[148] 随访时间更长的较近期研究表明,在 12 个月时,活动性方面的初始获益减少,[149] 在手术后 17 年时,完全丧失活动性,导致关节僵硬。[150] 关于 ADR 的长期益处和并发症,这些发现给出了一些提醒,尤其是在预防关节僵硬方面,[151][152][153] 使得将其作为一种治疗技术应用的普遍性下降。
[Figure caption and citation for the preceding image starts]: 椎间盘置换:患者表现为严重的背痛,先前因右侧骶 1 神经根病变已经接受了右侧腰 5 骶 1 椎间盘切除。 尽管初期康复,但右侧骶1疼痛及背痛在10个月后复发。 磁共振成像显示腰5骶1椎间盘退变(左,T2加权矢状位观)。 患者继而接受椎间盘置换术(前后位,右上,侧位,右下)。 背痛及右下肢痛彻底解除来自N.Quiraishi博士的收集 [Citation ends]. 这一装置的目的在于恢复椎间盘正常的动力学特征,缓解疼痛,同时避免失稳,并保护邻近关节突过度退变。置换整个椎间盘的原理是基于设计和用于其他关节(膝和髋关节置换)的类似假体置换取得成功。因此,所用的材料也是类似的(聚乙烯、铬、钴、钛)。人工椎间盘置换的应用指征包括:保守治疗失败;椎间盘退行性疾病致残的腰痛,累及不超过2个椎间盘。[146] 这些指征与脊柱融合的指征相似,但有一些注意事项(相对早期的关节突关节受累,无明显的失稳;如椎体滑脱)。 人工椎间盘置换的禁忌症包括狭窄,关节突关节炎,峡部裂或椎体滑脱,继发于突出椎间盘的神经根病变,硬化,骨质疏松,妊娠,肥胖,感染和骨折。[147] 人工椎间盘置换与融合手术在疗效和安全性上的对比已经有文献详细报道。 尽管最初的结果鼓励人工椎间盘的应用,[148] 随访时间更长的较近期研究表明,在 12 个月时,活动性方面的初始获益减少,[149] 在手术后 17 年时,完全丧失活动性,导致关节僵硬。[150] 关于 ADR 的长期益处和并发症,这些发现给出了一些提醒,尤其是在预防关节僵硬方面,[151][152][153] 使得将其作为一种治疗技术应用的普遍性下降。 